CJBMB: 40 Years of Biochemistry and Molecular Biology in China Multiple Myeloma I : From Bench Work to Clinical Management
ZHANG Chuan-Min, MEI Si-Jing, HAN Lei, SHI Yuan-Wei, XIAO Bo-Lian, XIE Xiao-Li, SU Quan-Ping
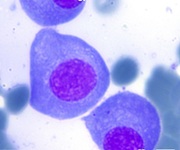
Although teniposide (VM26) is widely used in the treatment of lymphoma, its poor water solubility, low bioavailability and systemic toxicities still limit its clinical application. Nano-delivery systems are effective in increasing the bioavailability and reducing the toxicity of VM26, but there is an urgent need to overcome the problem of its non-specific targeting. Therefore, in this paper, we designed and constructed a hyaluronic acid-modified teniposide-targeted nano-delivery system (VM26-TNDS), and characterised its drug encapsulation rate, particle size and zeta potential. We also investigated the effects of VM26-TNDS on B-cell lymphoma cells with different expression of CD44 receptor, in terms of cellular targeting, inhibitory effect of proliferation, and induction of apoptosis and necrosis. The results showed that the drug encapsulation efficiency of VM26-TNDS exceeded 85%, and its liquid formulation could be stably stored at 4 ℃ for more than 6 months without precipitation. Based on CD44 receptor expression, Granta-519 (high expression), Raji (medium-low expression) and SU-DHL-4 (almost no expression) were screened for cellular experiments. Compared with VM26-NDS, the targeted modification could effectively reduce the uptake of VM26-TNDS by RAW264.7 and increase the uptake of VM26-TNDS by CD44 receptor-expressing lymphoma cells. The inhibitory proliferative effect and apoptotic necrosis-inducing ability of VM26-TNDS were stronger than those of VM26-NDS for Granta-519 and Raji cells, whereas there was no significant difference in the inhibitory effect on proliferation and ability to induce apoptosis and necrosis between VM26-NDS and VM26-TNDS in SU-DHL-4 cells, reflecting the targeting advantage for VM26-TNDS, as expected. However, its toxic effect on B-cell lymphoma cells only reflected the targeting advantage at some concentrations (0.25 μmol/L and 0.5 μmol/L), which met the expectation. The above results indicate that a teniposide-targeted nano-delivery system, VM26-TNDS, has been successfully prepared in this study. VM26-TNDS improves the delivery efficiency of VM26 by targeting human B-cell lymphoma cells expressing the CD44 receptor, thus killing human B-cell lymphoma cells more effectively and overcoming the problem of non-specific targeting in drug delivery to improve the therapeutic effect. Its biological therapeutic effects and mechanisms still need to be proved by more in vitro and in vivo experimental evidence.